Guillain-Barré syndrome (GBS) is a rare condition of the nervous system that can affect the movement and sensation in a person’s upper and lower limbs. This condition can be very distressing to go through. While there are effective treatment options available, and most patients will make a complete recovery, it can sometimes be a very debilitating disease leading to paralysis of the whole body.
Fortunately for many people looking for alternative treatments, there is plenty of potential in treating GBS by harnessing the regenerative potential of stem cells. This can provide hope for those facing more severe symptoms or delayed recovery from the condition.
In this article, we will look through the syndrome, its causes and symptoms, and the currently available treatments, including stem cell therapy.
Contact us
We provide free online consultations on the expected results of the treatment, its cost, and its duration. Learn about the opportunity of stem cell therapy for your particular case.

Medical Advisor, Swiss Medica doctor
What is Guillain-Barré syndrome and is it difficult to treat?
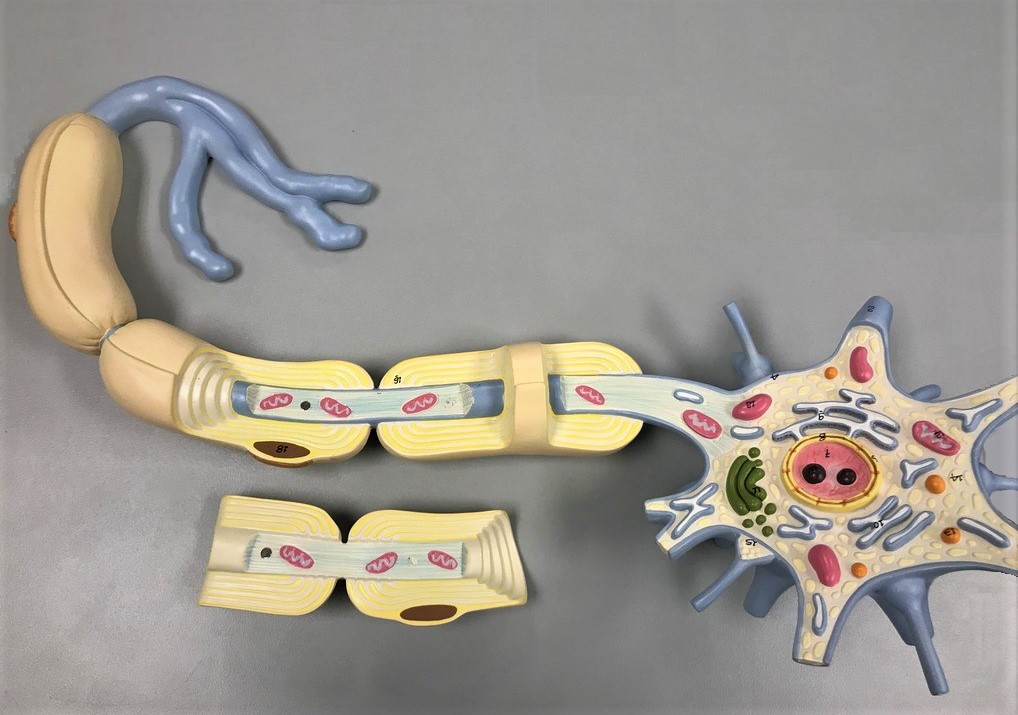
Guillain-Barré syndrome is a rare autoimmune condition that affects the nervous system. In this syndrome, the body’s immune system attacks the covering of the nerve cells, known as the myelin sheath, or attacks neurons directly (less common), which affects how these neurons are able to function. The most common form of GBS is also considered an acute inflammatory demyelinating polyradiculoneuropathy (AIDP).
While in most people, GBS usually resolves on its own, it can be potentially life-threatening at its most severe. Guillain-Barré syndrome is not difficult to treat only when it is targeted early enough. Treatment focuses on eliminating the immune cells which are attacking the nervous system to reduce the severity and progression of the condition.
Causes and symptoms of GBS
When the body undergoes a stressful situation such as illness or vaccination, the body’s immune cells fight the microorganism that has been introduced into the body. They produce antibodies against a certain antigen on this microorganism.
However, in some cases, the antigen on the microorganism is similar enough to the features of certain cells in the body. This is usually seen when the illness is a viral condition but can be seen in any of the following:
- Cytomegalovirus
- Epstein-Barr virus
- HIV
- Flu
- Dengue fever
- Zika virus
- Glandular fever
- Gastroenteritis from campylobacter bacteria
- Influenza vaccines
- Surgery
In the case of GBS, these antibodies are fooled into seeing the myelin sheath on the nerve cells and the antigen on the microorganism to be the same thing. As a result, they destroy the myelin sheath and the transmission of signals on these nerves is affected, and this causes the symptoms seen in GBS.

The most common symptoms seen in the early stages of Guillain-Barré syndrome include:
- Weakness in the limbs, particularly the legs
- Numbness
- A pins and needles sensation in the hands and feet
- Difficulty coordinating movements of the limbs
However, the symptoms will continue to get worse until about two to four weeks after the start of the condition, when they peak. The symptoms and signs that will be seen at this point in the progression of GBS are:
- Inability to walk or move the legs without assistance
- Facial paralysis
- Difficulty breathing
- Severe pain
- Change in heart rate
- Change in blood pressure
- Reduced bowel and bladder activity
- Blurred vision
Is Guillain-Barré syndrome curable?
There is no certain cure available for patients who are suffering from Guillain-Barré syndrome, and treatments only seek to manage and reduce the symptoms. With treatment, a person will most likely have milder symptoms for a shorter amount of time than someone without.
Ultimately, despite there being no cure, GBS is a self-limiting condition, which means that most individuals who have this syndrome will ultimately recover once it runs its course, even without treatment. However, in some patients, the syndrome may result in severe complications leading to disability and even death with a reported mortality rate of 3% to 13%.
Consequences of GBS
There are several different kinds of complications that people with GBS can face. These consequences are outlined below:
- Severe breathing difficulty: almost every third patient with GBS develops respiratory failure requiring intensive care unit admission and mechanical ventilation.
- Cardiovascular complications (arrhythmias, and variations in blood pressure).
- Infectious diseases (like pneumonia, sepsis, or meningitis).
- Blood clots and pulmonary embolism.
- Reduction in bowel and bladder activity.
- Bedsores (pressure sores).
- Relapse.
What are the common treatments for GBS?
There are two major kinds of treatment given to patients with GBS to help reduce the autoimmune damage being caused. These are therapeutic plasma exchange (plasmapheresis) and intravenous immunoglobulin (IVIG). Either of these treatments can be used for patients as they have been determined to have similar efficacy.
Supportive treatments can also be given to take care of symptoms the patient is having.
Therapeutic plasma exchange
Therapeutic plasma exchange, or plasmapheresis, is a treatment procedure that essentially cleanses the blood of the problematic antibodies that are attacking the nervous system.
The patient will be connected to a machine and their blood will pass through it several times. The machine will remove these antibodies before returning the blood back to the body.
Patients who receive this treatment will typically need several sessions of treatment for the best efficacy. The results of plasmapheresis for GBS were better and faster improvements in motor and respiratory functions.
Intravenous immunoglobulin
Receiving intravenous immunoglobulins is an alternative treatment to plasma exchange. Many patients may find this procedure preferable as it is less invasive than plasmapheresis and simply requires one port for intravenous access.
This procedure uses healthy antibodies from a donor and administers them intravenously to block the harmful antibodies from being able to destroy the nerves.
Supportive treatment
Patients receiving treatment for Guillain-Barré syndrome may also receive other forms of treatment such as analgesics to reduce their pain, and anticoagulants like heparin to reduce the risk of blood clots forming due to immobility.
Physical therapy helps with the weakness of their limbs and the disability experienced during recovery, and in more severe instances, a ventilator may be required to assist with respiration and a feeding tube if the patient finds it difficult to swallow or chew food.
Possible side effects
The treatments available for GBS are relatively safe. However, treatment with plasma exchange comes with a small risk of relapse within the first six to twelve months following the onset of the disease when compared to those who received no treatment, despite the achieved improvements.
With intravenous immunoglobulins, there are quite a few side effects that patients can experience, but most patients experience mild effects, which tend to be flu-like. They include the following:
- Fever
- Chills
- Headache
- Fatigue
- Nausea
Moderate and severe adverse reactions to IVIG include dermatological effects like hives (urticaria), eczema, dermatitis, and papules. In rarer instances, patients can experience cardiovascular side effects like low blood pressure and arrhythmias.
Stem cell therapy – an alternative treatment of Guillain-Barré syndrome
Stem cell therapy is one of the most promising alternative treatments for patients who are not satisfied with the results that they are getting from more conventional measures. It can also be combined with these measures.
It has been proven that the use of adult stem cells in the treatment of conditions like GBS can halt progression in as many as two-thirds of patients, with the return of normal motor and sensory function that has been lost.
Learn how it works
Animal studies have shown that specimens with defective myelination improved and developed myelin sheaths in as little as five weeks following the administration of stem cells. A similar effect was seen in another animal study, but myelination was seen in just about 14 days.
It has also been proven that neurons in the peripheral nervous system can be repaired through the transplantation of stem cells harvested from the adipose tissue, and these results can be seen in just two weeks after they are administered.
Another means by which a stem cell transplant can improve GBS is through immune modulation. Since immune dysfunction is at the core of this condition, the natural tendency of stem cells in suppressing immune cells to help overcome pathological inflammatory processes is very beneficial.
What is the procedure?
Administering stem cells for Guillain-Barré syndrome is quite a straightforward process for the majority of patients. The stem cells will be harvested from the patient or a compatible donor and they will be prepared for administration.
After local anesthesia to numb the point of injection, the patient will have an intravenous drip inserted into a vein, through which the prepared stem cell infusion will be passed into the bloodstream. Several procedures may require to achieve a sustainable and significant treatment result.
There may be mild pain following the procedure at the point of injection, but besides that, side effects are very minimal.
How long does the recovery take in GBS?
The time it takes for a patient to recover from GBS varies significantly. For most patients, recovery will take anywhere between four to twelve months, depending on the severity of symptoms. Four out of every five patients will be able to walk on their own six months after the disease started.
However, in some instances, it can take individuals who have had GBS several years to fully recover. Stem cell therapy alone or in combination with complementary therapies can increase the rate of recovery and improvement.
How to enter the treatment program, and what it may include
Entering the stem cell treatment program for Guillain-Barré syndrome starts by contacting our facility by phone or email. Your free online consultation will answer all the questions you have about what to expect from the treatment, how much it will cost, and how long the treatment will take.
When you come for stem cell therapy for GBS at Swiss Medica, you will receive the most holistic care to target the condition completely, beyond just stem cell infusions.
Treatment will always begin with a consultation and appropriate tests, which help ascertain a patient’s full medical history, any treatments they might have received prior, and an evaluation of their physiology and the state and severity of the disease. All this makes it possible to tailor a personalized and effective treatment plan for the patient.
In the case of GBS, besides stem cell treatment, patients may receive other forms of care to ensure that their treatment and recovery are as optimal as possible. This will include physical therapy, plasmapheresis, and pain control. Some patients may also benefit from monitoring vitals like heart rate, blood pressure, and respiration, particularly when they have severe symptoms, and assistance provided by the Clinic’s medical staff for these problems.
Get a free online consultation.
Contact us to learn about the cost and duration of the treatment program for GBS, what it may involve, and what are the expected results for your case.

Medical Advisor, Swiss Medica doctor
Quellenangaben:
Mukerji, S., Aloka, F., Farooq, M. U., Kassab, M. Y., & Abela, G. S. (2009). Cardiovascular complications of the Guillain-Barré syndrome. The American journal of cardiology, 104(10), 1452–1455.
Bianca van den Berg, Carina Bunschoten, Pieter A. van Doorn, Bart C. Jacobs. Mortality in Guillain-Barré syndrome. Neurology, Apr 2013, 80 (18) 1650-1654.
Shang, P., Zhu, M., Baker, M., Feng, J., Zhou, C., & Zhang, H. L. (2020). Mechanical ventilation in Guillain-Barré syndrome. Expert review of clinical immunology, 16(11), 1053–1064.
Anders, J., Heinemann, A., Leffmann, C., Leutenegger, M., Pröfener, F., & von Renteln-Kruse, W. (2010). Decubitus ulcers: pathophysiology and primary prevention. Deutsches Arzteblatt international, 107(21), 371–382.
Bĕlohlávek, J., Dytrych, V., & Linhart, A. (2013). Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism. Experimental and clinical cardiology, 18(2), 129–138.
Raphaël, J. C., Chevret, S., Hughes, R. A., & Annane, D. (2002). Plasma exchange for Guillain-Barré syndrome. The Cochrane database of systematic reviews, (2), CD001798.
Ortiz-Salas, P., Velez-Van-Meerbeke, A., Galvis-Gomez, C. A., & Rodriguez Q, J. H. (2016). Human Immunoglobulin Versus Plasmapheresis in Guillain-Barre Syndrome and Myasthenia Gravis: A Meta-Analysis. Journal of clinical neuromuscular disease, 18(1), 1–11.
Wijdicks, E. F., & Ropper, A. H. (1990). Acute relapsing Guillain-Barré syndrome after long asymptomatic intervals. Archives of Neurology, 47(1), 82–84.
Guo, Y., Tian, X., Wang, X., & Xiao, Z. (2018). Adverse Effects of Immunoglobulin Therapy. Frontiers in immunology, 9, 1299.
Uchida, N., Chen, K., Dohse, M., Hansen, K. D., Dean, J., Buser, J. R., Riddle, A., Beardsley, D. J., Wan, Y., Gong, X., Nguyen, T., Cummings, B. J., Anderson, A. J., Tamaki, S. J., Tsukamoto, A., Weissman, I. L., Matsumoto, S. G., Sherman, L. S., Kroenke, C. D., & Back, S. A. (2012). Human neural stem cells induce functional myelination in mice with severe dysmyelination. Science Translational Medicine, (2012) 4, (165er7).
Keilhoff, G., Stang, F., Goihl, A., Wolf, G., & Fansa, H. (2006). Transdifferentiated mesenchymal stem cells as alternative therapy in supporting nerve regeneration and myelination. Cellular and molecular neurobiology, 26(7-8), 1235–1252.
Di Summa, P. G., Kingham, P. J., Raffoul, W., Wiberg, M., Terenghi, G., & Kalbermatten, D. F. (2010). Adipose-derived stem cells enhance peripheral nerve regeneration. Journal of plastic, reconstructive & aesthetic surgery: JPRAS, 63(9), 1544–1552.
Young, H.E., Speight, M.O. (2021). An Alternative Novel Therapy for the Treatment of Chronic Inflammatory Demyelinating Polyneuropathy: Adult Autologous Telomerase-Positive Stem Cells. Stem cell & regenerative medicine, 5(2), 1-16.
Jiang, W., & Xu, J. (2020). Immune modulation by mesenchymal stem cells. Cell proliferation, 53(1), e12712.