Introduction
The liver is the fundamental visceral organ, the largest gland and third largest organ in the body after skin and the intestines. While it is widely assumed to be part of the digestive system, it fulfills about 500 functions, including detoxification, the maintenance of energy levels, the metabolism of fats, participation in blood production, production of amino acids and regulation of blood clotting.
More information on liver function can be found in this video:
Currently, there is no effective curative option for cirrhosis, and all approaches available are only aimed at symptom management with various severe side effects.
Stem cell transplantation can stimulate the inherent regenerative capacity of the liver through mild but significant change in the liver tissue microenvironment, and it can improve the liver function. Among other stem cells, mesenchymal stem cells (MSCs) have demonstrated impressive therapeutic potential for treating various diseases, including those of the central nervous system as well as musculoskeletal and autoimmune disorders.
What Is Liver Cirrhosis?
Cirrhosis of the liver is when the normal tissue of the liver is replaced with scar tissue due to various liver injuries. This process results in the progressive loss of liver function as the repaired areas are composed of fibrous bands and nodules rather than hepatocytes and other functional cells.
The majority of the healthy liver (60-80%) is made up of liver cells called hepatocytes. These cells have an average lifespan of 150-250 days, which means that the liver is constantly renewing itself under normal conditions. It is the only organ in the body that can easily replace damaged cells, but if enough cells are lost, the liver may not be able to meet the needs of the body which leads to liver failure.
The liver is a regenerative organ, but it is limited in this ability depending on the energy reserve needed to heal and the host of responsibilities that must be attended to daily regardless of this central organ’s ability to keep up the pace.
Liver disease can progress to cirrhosis and liver failure. Associated complications include increased risk of bleeding and infection, malnutrition and weight loss, decreased cognitive function over time and an increased risk of cancer.
Reinforcing therapies, such as stem cell treatment, can transfer patients from a condition of day-to-day survival to ones in which they feel a better quality of life.
Causes of Liver Cirrhosis
Although the term ‘cirrhosis’ covers multiple conditions that lead to liver damage, there are a considerable amount of underlying causes of such conditions. The most common are the following:
- Alcoholic liver disease (liver impairment caused by alcohol overuse)
- Nonalcoholic fatty liver disease (accumulation of fat in the liver)
- Chronic hepatitis C or B
There are other less frequent causes of cirrhosis, which include heredity and autoimmune and chronic medical conditions, such as:
- Primary liver cancer
- Primary biliary cirrhosis
- Primary sclerosing cholangitis
- Long-lasting use of specific pharmaceutical products
- Budd-Chiari syndrome
- Hemochromatosis
- Wilson’s disease
- Transthyretin-related amyloidosis
- Gilbert’s syndrome
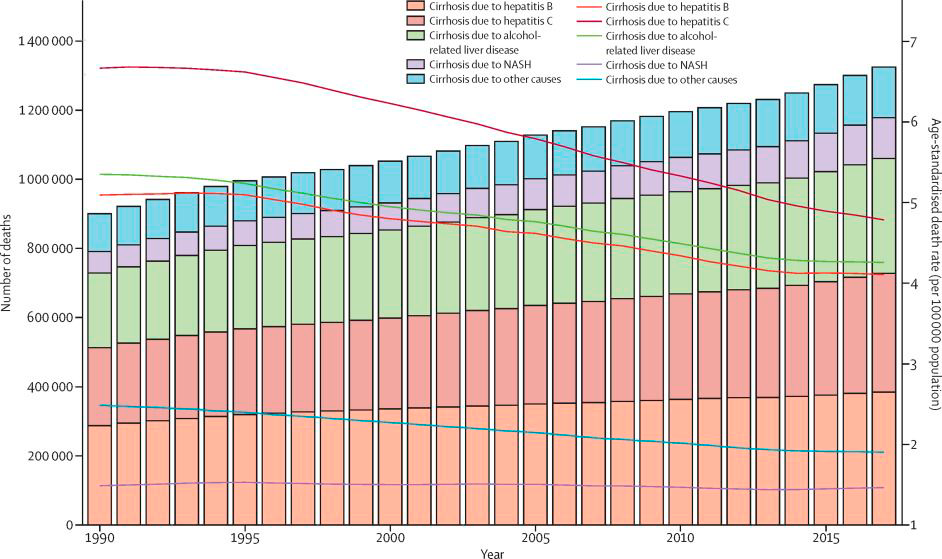
Bars refer to the number of deaths in each year. Lines refer to age-standardized death rate each year. NASH = non-alcoholic steatohepatitis.
Current Approaches to Treatment of Liver Cirrhosis
Although the liver can be recovered, there are no warning signs that it is failing until it is too late. Once the line is crossed between chronic liver disease and the final stage of liver failure, there are fewer options. Up to now, there is no liver dialysis that can rehabilitate liver function in the way that kidney failure is treated. Transplantation is currently the only effective treatment for liver failure, but it has many drawbacks, including the risk of rejection, risks associated with surgery and a shortage of donors.
Patients with cirrhosis should do their best not to allow deterioration and progression of their condition. This means maintaining a healthy diet and body weight through regular physical activity, absolute abstinence from alcohol, caution with medications, regular blood tests and getting screened for liver cancer. A healthy lifestyle facilitates a reduction of fat in the organ, and it decreases inflammation and scarring of the liver tissue.
In the initial stages, patients are not aware of their disease and have no symptoms, or their symptoms are so mild that they provide no clues to the hidden destructive processes happening within them. Such cirrhosis is described as compensated, and in most cases, it is revealed accidentally during medical examinations or tests prescribed for other reasons.
As the cirrhosis progresses, more frequent medical visits, prolonged hospitalization and an increasing amount of medication are required. It affects both quality of life and financial status.
Treatment approaches vary depending on the causes and the type of cirrhosis and its already-existing complications.
| CAUSES AND COMPLICATIONS OF CIRRHOSIS | |
| Causes | Treatment |
| Alcoholic liver disease | Complete abstinence from alcohol. Treatment of alcohol abuse (behavioral treatments, medications, support groups). |
| Nonalcoholic fatty liver disease | Healthy diet and regular physical activity. |
| Chronic hepatitis C and B | Corresponding antiviral medicines. |
| Autoimmune hepatitis | Immunosuppressive drugs. |
| Diseases that affect bile ducts (primary biliary cholangitis, primary sclerosing cholangitis) | Surgical procedures to open narrowed or blocked bile ducts. Medications that dissolve gallstones and/or prevent formation of gallstones. |
| Inherited liver diseases | Managing symptoms and complications. |
| Long-term use of medicines | Discontinuation of certain drugs. |
| Complications | Treatment |
| Portal hypertension (vascular disease of the liver) | Drugs that lower high blood pressure in the portal vein. Removal of fluid accumulated inside the abdominal cavity (ascites) through the use of medications and/or physical drainage. |
| Hepatic encephalopathy | Drugs that lower the levels of toxins in the brain and improve brain function. |
| Bacterial infections | Antibiotics. |
| Liver cancer | Surgery, radiation therapy, chemotherapy, liver transplant. |
| Liver failure (end-stage liver disease) | Liver transplant. |
However, the body is so exhausted by the chronic disease that it hardly sustains another burden of medication as the drugs are mostly utilized by the liver, and adverse events of such treatment are frequent and severe. The queue for liver transplantation is quite long, and not all candidates are healthy enough to undergo the procedure. Although dozens of patients with acute liver failure have received donated hepatocyte transplants with some improvement in liver function, the effects are not often significant.
Stem Cells for Liver Cirrhosis
Stem cells are actively being studied as a favorable alternative for the current treatment options. Due to the natural mode of action, stem cells provide mild but sustained results for patients.
Various types of stem cells were studied in vitro, however, not all of them are suitable for human use. The following cells have become commonly utilized in studies and clinical practice in humans:
- Hematopoietic stem cells (HSCs) are derived from bone marrow and umbilical cords. For several decades these cells have helped to cure blood disorders.
- Hepatic progenitor cells (HPCs) are located in the liver normally and serve as the source for liver tissue recovery. However, they are suspected to play a part in liver tumor growth.
- Mesenchymal stem cells (MSCs) are adult stem cells found in many organs and tissues. They are the most prospective and safest candidates for cell-based therapies.
Mechanism of Stem Cell Activity
MSCs are the “frontrunner” for clinical practice due to the following advantages:
- Different sources for MSCs isolation
- Capability for large-scale production
- Ability to transform into a variety of cell types in experimental models
- Ability to migrate toward damaged tissues
- Multiple therapeutic effects: anti-inflammatory, immunomodulatory, anti-apoptotic, anti-fibrotic and angiogenic
The overall benefits of MSCs result in restoration of lost tissue functions and increasing the regeneration potential of the body.
The benefits of MSCs make them suitable for the treatment of pathologies like neurological and autoimmune diseases, diabetes, musculoskeletal problems and others.
Scientific Basis for Using Stem Cells in Treating Patients with Liver Cirrhosis
The application of stem cells of different types and from various sources in healing liver injuries has been studied for about 20 years. The feasibility of using stem cells for combating cirrhosis and its complications were confirmed both in model and clinical studies.
MSCs act through producing various growth factors and cytokines that, among other functions, stimulate liver recovery by activating the body’s own stem cells, reviving hepatocytes.
The ability of transplant MSCs to engraft into host livers and contribute to improvement of fibrosis has been demonstrated in animal models. It was also shown that MSCs suppress the function of hepatic stellate cells which play a key role in fibrosis (formation of scar tissue). Besides the downregulation of fibrogenic activity, MSCs reduce inflammatory levels and stimulate proliferation of hepatocytes.
Expected Results: What Improvements Do Patients Get?
The hepatoprotective and immunomodulating properties of stem cell-based therapy can help combat symptoms of cirrhosis such as fatigue, intestinal issues, weight loss, skin disorders and jaundice (yellow discoloration of the skin and whites of the eyes). Stem cells also contribute to the acceleration and intensification of regeneration processes in the damaged tissues. The overall health-protecting effect increases energy levels and improves quality of life.
Factors such as age, hereditary predisposition, the stage of the illness and the severity of symptoms may alter the effectiveness of cell-based therapy. Thus, each case is individual, and the results of the therapy cannot be standard. Also, applying only stem cells for some cases may not be enough. Cell therapy works more effectively when combined with other therapeutic methods that help activate the tissue repair process.
Contact us
Get a free online consultation with a medical advisor to find out how stem cells would benefit your case.

Medical Advisor, Swiss Medica doctor
Patient Outcomes and Testimonials of Liver Cirrhosis Treated with Stem Cells at Swiss Medica
One of our patients, Oscar from the United States, shared his impressions of a visit to Swiss Medica. He was treated for liver cirrhosis in a Russian branch of the clinic. He spent 12 days at Swiss Medica’s clinic in Moscow and felt “great, amazing”. Watch the video testimonial here (in Spanish with English subtitles):
Liver Cirrhosis Treatment with Stem Cells: The Procedure
Prior to any treatment procedures, specialists of Swiss Medica conduct a comprehensive study of the patient’s medical history and current health status. This includes a physical examination, blood and urine diagnostic tests and a consultation with the necessary specialists. This approach allows our doctors to set targets for using cell therapy and choose the most profitable type of cell product.
Cell products for the treatment of liver cirrhosis can be prepared from an autologous material, i.e.,the tissues of the patient (bone marrow and/or fat tissue). In this case, cell cultivation takes about 3-4 weeks. Besides, Swiss Medica has its own bank of donor cells which also may be used alone or together with autologous cells. Using donor (allogeneic) cell products is recommended when the therapy should start immediately or in cases when it is impossible to use the patient’s own biomaterial for objective reasons.
If no contraindications are revealed and the patient is eligible for stem cell therapy, the therapy may be started. Basically, it includes 4 steps:
- Sampling (harvesting) of biomaterial
- Stem cell isolation and further cultivation (growing to the required amount)
- Cell product activation
- Cell product administration
The steps which suppose the involvement of the patient (sampling of biomaterial and administration of cell product) are executed under full medical control (monitoring of ECG, heart rate, respiratory rate, blood pressure, oxygen saturation level).
Treatment protocols may include the use of donor cells, so there is no need to perform manipulations to take the patient’s own cells. This also shortens the period before starting treatment (as it reduces the time expected for cultivation) and does not require repeated visits to the clinic.
Read more information about stem cell treatment procedures here.
Optionally, the patient may be prescribed the following rehabilitation procedures to help activate the tissue repair process after the introduction of stem cells introduction:
- Xenon gas rehabilitation therapy (inhalation procedure)
- IMR therapy
- Ozone-laser injection therapy
- Cryotherapy
Is the Treatment Safe and Are There Any Side Effects?
According to the vast majority of the data currently available, the use of MSCs is safe in patients with liver cirrhosis as well as in those with other pathologies. The meta-analysis of the safety of MSCs in clinical trials has shown that no serious side effects were associated with injection of both autologous and allogeneic MSCs. Patients reported a short-term fever as the most common adverse side effect of treatment with stem cells. This phenomenon occurs without complications and passes on its own.
In general, therapeutic benefits from the use of products based on patients’ own (autologous) or donated MSCs for liver cirrhosis include:
- Slowing or stopping the destructive process in the tissues of the body
- Systemic positive effects from stem cells (rejuvenation of the body, increased energy levels, improved well-being, alleviation of the symptoms of cirrhosis and other related diseases)
- Improving regenerative capacity of the body
- Increasing quality and length of life
Get a free online consultation
Contact us to learn about the expected results of the treatment, its cost and duration.

Medical Advisor, Swiss Medica doctor